Automate
your claims processing workflows with accuracy
Exceptional accuracy
AI Agents process 200+ document types for Direct Mortgage Corp, leading to a 20x faster application approval process.
Easily access healthcare data
Reduce response times by 90%+ and provide data-driven answers to any queries using AI Agents.
Your data, your infrastructure
80%
15%
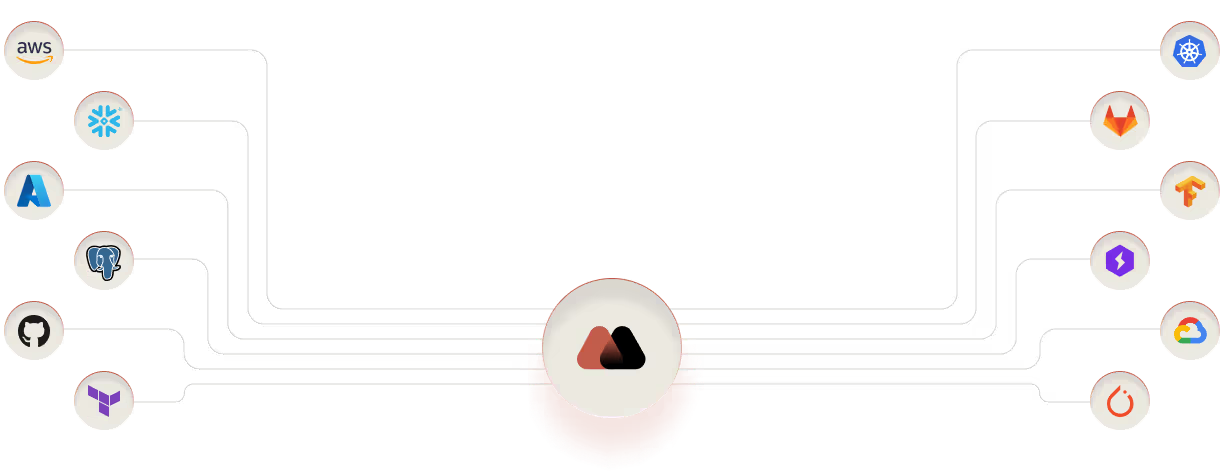
Your data should never leave your walls.
With software deployed on your private infrastructure, access stays strictly in-house.
.avif)
Custom LLM training
80%
15%
We train our AI Agents on your documents and data, so they’re ready to handle your verification tasks as soon as you adopt them.

AI Agents enhance healthcare operations and minimize costs
97%
40x
80%
20%
Boost Patient Satisfaction
AI Agents accelerate the approval process, reducing wait times for treatments.
Reduce Denial Rates
Ensure all necessary criteria are met before submission to drastically lower the chance of claim denials.
Maintain Compliance
Keep your healthcare business legal by complying with regulations like the HIPAA and GDPR.
Support Clinical Decision-Making
AI analyzes hundreds of data points to make better decisions regarding patient care plans.
Optimize Health Outcomes
Ensure timely approvals for necessary procedures and medications using AI Agents.
Scale Operations Efficiently
Handle large volumes of prior authorizations simultaneously without expanding your team.
How it works

Extract patient data in custom fields
Document AI extracts information like insurance details, medical histories, and patient identifiers.

Make informed, accurate prior authorization decisions
Decision AI evaluates multiple data points, including medical histories and treatment protocols to provide reliable decision support.

Retrieve key information from your databases
It delivers this information through the form of natural language responses through a chat-like interface.

Provide superior patient and staff support
They return this information in the form of natural language responses.

See automated prior authorization in action
See how our AI Agents work live before you commit. Schedule a free, 30-minute consultation today.
See how AI Agents work in real time
Learn how to apply them to your business
Discuss pricing & project roadmap
Get answers to all your questions
Leave no questions unanswered
What is electronic prior authorization and how does AI improve its efficiency?
Electronic prior authorization (ePA) uses digital systems to submit and process prior authorization requests electronically instead of using traditional paper forms or manual entries. AI enhances ePA by:
- Reducing errors
- Automating data extraction
- Speeding up decision-making
This leads to faster approvals so patients retrieve timely medical care, speeding up the prior authorization process. It also boosts workflow efficiency by saving time and reducing operational costs.
What benefits do automated prior authorization solutions provide and do they integrate with electronic health records (EHRs)?
Prior authorization automation solutions seamlessly integrate with existing electronic health records (EHRs) systems, as well as:
- Extract relevant patient data directly from EHRs
- Populate prior authorization forms
- Submit the forms to insurers without manual intervention
As a result, these solutions reduce the amount of administrative tasks for healthcare providers so staff can focus more on delivering high-quality patient care instead.
Can AI help in monitoring prior authorization metrics effectively?
Yes, AI plays an important role in monitoring and analyzing certain prior authorization metrics. A prior authorization solution can track and analyze data on approval rates, processing times, and denial reasons. This provides healthcare providers with actionable insights to make more informed prior authorization decisions in less time.
What are the benefits of using AI to manage prior authorization submissions for healthcare providers?
One key benefit is automating various aspects of prior authorization submission management, including:
- Identification and extraction of necessary patient and treatment information
- Submitting requests directly to insurers
- Tracking the status of these submissions
This reduces administrative load, minimizes delays in patient care, and helps healthcare providers focus more on patient treatment rather than paperwork.
How does automating prior authorization reduce healthcare costs and administrative burdens for health care organizations?
Automating prior authorization eliminates manual processes and accelerates approvals, so health care organizations can allocate resources more efficiently and focus on enhanced patient care. This leads to reduced overall operational expenses and boosts productivity by freeing up time for healthcare staff.
Can automated prior authorization solutions integrate with electronic health records to improve revenue cycle management?
Automated prior authorization solutions seamlessly integrate with electronic health records (EHRs), improving revenue cycle management by handling billing and insurance-related processes efficiently. It helps minimize delays in the revenue cycle, allowing for quicker reimbursements and reduced financial discrepancies within healthcare practices.
Can intelligent automation in prior authorization positively impact patient care and reduce negative patient outcomes?
Intelligent automation helps to speed up approval of necessary treatments, which directly improves patient care and reduces negative patient outcomes. It means authorization requests are processed quickly and accurately, letting patients gain access to needed medical services without unnecessary delays for improved overall health outcomes.
.svg)
.svg)

.avif)

